This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
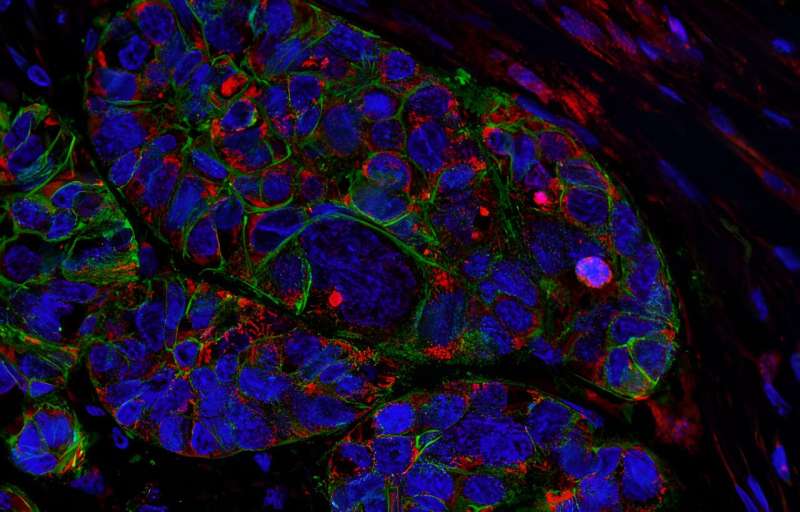
Attacking the roots of pancreatic cancer
Pancreatic cancer is not just one disease, but that's the way it is currently treated. New work from Tannishtha Reya's lab could help pave the way for a change. The research is published in the journal Cancer Cell.
Though most pancreatic cancers are classified as pancreatic ductal adenocarcinoma (PDAC), several other subtypes exist.
"Everyone gets the same chemotherapy, even though some subtypes are dramatically less responsive to the treatment and even more lethal," says Tannishtha Reya, Ph.D., the Herbert and Florence Irving Professor of Basic Cancer Science (in Physiology & Cellular Biophysics) at Columbia University's Vagelos College of Physicians and Surgeons and associate director of translational research at the Herbert Irving Comprehensive Cancer Center.
Because of the lack of relevant models and a poor understanding of the different forms of pancreas cancer, tumor subtype information is not taken into account for risk stratification or treatment.
Her findings—which reveal how a single pool of stem and progenitor cells in the pancreas can give rise to many different types of pancreatic cancer—should help researchers better understand the molecular underpinnings of each type and develop therapies that are better matched to an individual's disease.
Tracing the origins of pancreatic cancer
"Understanding the cell from which a cancer arises can allow you to trace how it progresses and the pathways it depends on to transition from a benign state to an aggressive malignancy," Reya says.
Her previous research in cancer development had found that the MSI2 gene, which encodes a protein that keeps cells in a "stem-like" state, is a key factor driving the aggressive nature of pancreatic cancers.
Reya's team, working with international collaborators, believed that the cancers could originate from stem cells in the pancreas that already express high levels of MSI2. What could cause these stem cells—normally reliable workhorses of tissue regeneration—to become cancerous?
Suspecting that mutations in another gene might trigger that transformation, Reya's team developed a genetically engineered model in which a mutated copy of the MYC gene, a well-known cancer inducer, was expressed exclusively in MSI2-expressing cells.
The test animals developed PDAC, the commonly studied form of pancreatic cancer, but also many other types, including adenosquamous carcinoma of the pancreas, acinar cell carcinoma, and anaplastic (undifferentiated) tumors.
The findings establish the MSI2-expressing cells as cells of origin for multiple types of pancreatic cancer and the first models of adenosquamous carcinoma, the deadliest form of the disease.
"This will allow us to better study how different subtypes arise and progress, how cells go from being normal to pre-cancerous, and how pre-cancer cells progress to end-stage diseases of different subtypes," says Reya. "This is also important because adenosquamous cells can be mixed in with PDAC in the human disease and these cells remain behind after current treatments. Thus, this model could be critical for understanding the most aggressive types of pancreatic cancer and finding ways to prevent its growth and recurrence."
Earlier detection?
The new model could also help physicians find pancreatic cancer early—an important goal for a disease that typically remains hidden well into its advanced stages. Finding the inflection point that causes a benign precancerous cell to become malignant, Reya says, could lead to new early detection and interception strategies.
Reya's team also hopes to use the new model to search for better treatments. They have already identified potential targets for new pancreatic cancer therapies, especially for types that resist current treatments. The researchers are investigating less conventional strategies as well, such as using late-stage cancer gene products as vaccines, causing the immune system to attack early-stage tumors before they get out of control.
More information: Nirakar Rajbhandari et al, Single-cell mapping identifies MSI+ cells as a common origin for diverse subtypes of pancreatic cancer, Cancer Cell (2023). DOI: 10.1016/j.ccell.2023.09.008


















